HIPAA compliance is not limited to hospitals and doctors. Anyone who touches protected health information as part of healthcare operations inherits responsibility, whether they realize it or not.
Most HIPAA failures happen because organizations assume compliance belongs to someone else.
At Mindcore Technologies, investigations repeatedly show the same root cause: PHI flows across organizations, systems, and vendors, but accountability stops at the wrong boundary. HIPAA rules exist to prevent that gap.
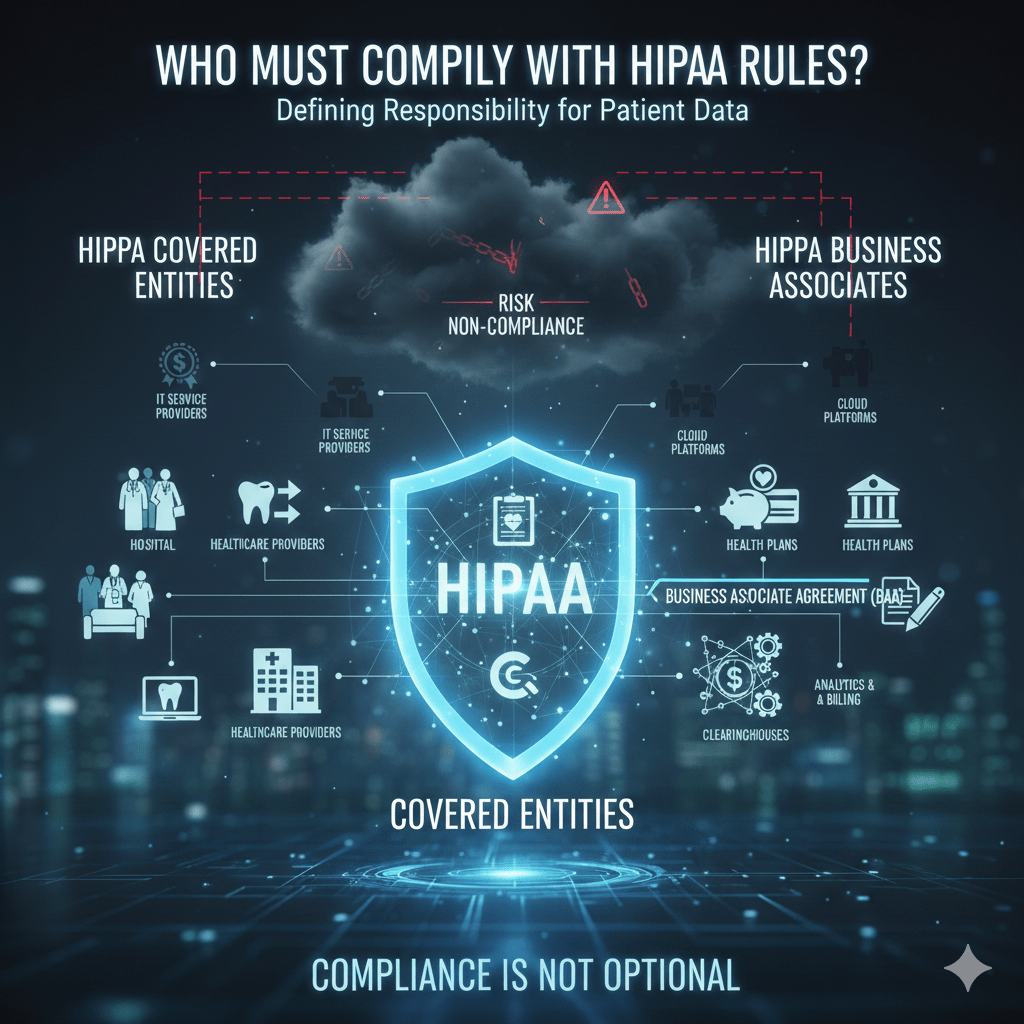
The Two Groups That Must Comply With HIPAA
HIPAA applies directly to two categories of organizations. If you fall into either one, compliance is not optional.
1. HIPAA Covered Entities
Covered entities are organizations that deliver, pay for, or administer healthcare and handle PHI as part of those activities.
Covered entities include:
- Healthcare providers
Hospitals, clinics, physicians, behavioral health providers, dentists, and telehealth providers that transmit health information electronically. - Health plans
Insurance companies, employer-sponsored health plans, Medicare, Medicaid, and prescription drug plans. - Healthcare clearinghouses
Organizations that process health information between providers and payers, such as billing and claims processors.
Covered entities carry primary responsibility for HIPAA compliance and patient data protection.
2. HIPAA Business Associates
Business associates are organizations or individuals that create, receive, maintain, or transmit PHI on behalf of a covered entity.
Common business associates include:
- IT service providers and managed service providers
- Cloud hosting and SaaS platforms
- Billing and revenue cycle management vendors
- Data analytics, transcription, and reporting services
- Legal, accounting, and consulting firms handling PHI
Business associates are legally required to comply with HIPAA through Business Associate Agreements, or BAAs.
Why Business Associates Are Directly Accountable
A common misconception is that business associates are only indirectly responsible.
That is false.
Business associates must comply with:
- HIPAA Security Rule safeguards
Administrative, physical, and technical controls protecting ePHI. - Breach notification requirements
Timely reporting of incidents involving PHI. - Limits on PHI use and disclosure
Access must align strictly with contracted purposes.
If a business associate causes a breach, regulators pursue both parties.
What HIPAA Compliance Actually Requires
HIPAA does not mandate specific tools. It mandates outcomes.
Organizations subject to HIPAA must be able to show:
- PHI access is limited to minimum necessary use
Users see only what their role requires. - Access is controlled and auditable
Activity can be traced and reviewed. - PHI is protected against unauthorized access or disclosure
Across systems, users, and vendors. - Incidents are detected and reported appropriately
Delays increase penalties and exposure.
Compliance depends on how access and data flow are designed.
Who Often Overlooks Their HIPAA Obligation
HIPAA compliance is frequently missed by:
- Technology vendors handling PHI indirectly
Especially cloud platforms and integration providers. - Third-party consultants and contractors
Temporary access still counts as PHI access. - Remote workforce providers
Home access does not reduce responsibility. - Subsidiaries and affiliates
Organizational structure does not negate compliance.
HIPAA applies based on function, not job title or contract language.
Why HIPAA Responsibility Cannot Be Outsourced
Covered entities often assume vendors absorb all risk.
In reality:
- Covered entities remain accountable for how PHI is accessed
- Vendor breaches still trigger covered entity obligations
- Poor vendor governance becomes a compliance failure
HIPAA expects organizations to govern PHI end to end, not delegate trust.
How Architecture Determines HIPAA Compliance
Organizations comply with HIPAA more effectively when:
- Access is identity-based, not network-based
- Permissions reflect job roles and purpose
- Sessions are limited and continuously monitored
- PHI stays inside controlled environments
- Vendor access is scoped and auditable
They struggle when access is broad, persistent, and difficult to track.
How Mindcore Technologies Helps Organizations Meet HIPAA Obligations
Mindcore helps organizations that must comply with HIPAA by:
- Identifying all PHI access paths
Including vendors, remote staff, and cloud platforms. - Reducing excessive access through identity-driven controls
Enforcing least privilege consistently. - Containing PHI inside secure access environments
Limiting endpoint and vendor exposure. - Improving audit readiness across organizations
Making compliance provable, not assumed.
The focus is reducing shared risk, not shifting blame.
A Simple HIPAA Responsibility Reality Check
You must comply with HIPAA if:
- You create, access, store, or transmit PHI
- You support healthcare operations involving PHI
- You provide IT, cloud, or analytics services touching PHI
- You can view or manage patient data, even temporarily
Intent does not matter. Access does.
Final Takeaway
HIPAA compliance applies to any organization that touches patient data as part of healthcare operations, not just care providers.
Organizations that understand this design access, vendor relationships, and data protection intentionally. Those that do not discover their responsibility only after audits, penalties, or breaches force the issue.